Francesco Prati, Flavio Giuseppe Biccirè
Updated on May 13, 2021
Drug-coated balloons (DCB) are gaining attraction worldwide for the treatment of peripheral and coronary lesions. The basic prerequisite for this therapy is the best possible lesion preparation. DCBs cannot replace drug-eluting stents, but will play an important role in the reduction of permanent implants in interventional vascular medicine in the future.
Andreas Grüntzig introduced coronary angioplasty into clinical use in 1977 . For the field of coronary interventions, the introduction of stents represented a major milestone. Stenting overcomes the major limitations of balloon angioplasty, namely, acute recoil, dissections, abrupt vessel closure and longer-term negative vessel remodelling. However, restenosis may be accelerated due to continued or increased neointimal proliferation associated with the permanent implant. Local intravascular drug delivery by drug-eluting stents (DES) that elute paclitaxel, sirolimus, or their associated analogues have successfully addressed this cellular basis of restenosis in the coronary territory. However, delayed or incomplete re-endothelialisation with the need for long-term dual antiplatelet therapy (DAPT) to reduce the risk of stent thrombosis can limit the use of this technology. Sustained drug release seems to be essential for stent-based local drug delivery because of the inhomogeneous drug distribution from a DES to the arterial wall , with the consequence of delayed and incomplete re-endothelialisation of the stent struts . Even with the latest generation of DES, device-associated annual event rates of 2 to 3 % are seen beyond the first year , . The risk of long-term events increases with the number and length of DES . Therefore, new alternative concepts aim at local drug delivery without permanent scaffolding.
Antiproliferative agents such as paclitaxel are suitable for the prevention of local intravascular restenosis due to their high lipophilicity and tight binding to various cell constituents . The addition of a contrast agent surprisingly resulted in a solubility of paclitaxel and its analogues far beyond the concentrations applied in previous investigations . In the porcine coronary model, the intracoronary bolus administration of a taxane-contrast medium formulation led to a significant reduction of neointimal formation after experimental coronary stent implantation despite the short application time , . Paclitaxel in a contrast agent was better tolerated and led to higher local tissue concentrations than diluted Taxol, indicating the impact of additional compounds for local drug transfer . The surprising discovery was that sustained drug release is not a precondition for long-lasting restenosis inhibition.
In 2001, the basic premise of a more lesion- than vessel-specific method of intramural drug delivery became embodied in the concept of a drug-coated balloon (DCB) . By coating paclitaxel onto the surface of a conventional angioplasty balloon an effective local drug concentration is achieved with very low systemic exposure. After the clinical proof of efficacy was provided a few years later , the concept of DCB is considered a milestone in interventional cardiology , .
The basic in vitro and in vivo experiments that lead to the concept of DCB identified a specific matrix coating with paclitaxel in combination with a small amount of the hydrophilic X-ray contrast medium iopromide (Paccocath™) (Figure 1, Figure 2) . The balloons were angioplasty balloons coated with a paclitaxel dose between 1.3 and 3 μg/mm2 of balloon surface. At 1-month follow-up, the implantation of stents premounted on paclitaxel-coated balloons was found to have significant, dose-dependent reduction in angiographic late lumen loss (LLL) and a statistically significant increase in minimal lumen diameter compared with controls. Histomorphometry showed a statistically significant increase in lumen diameter and lumen area and a corresponding decrease in maximal neointimal thickness and neointimal area in the vessels treated with paclitaxel-coated balloons (Figure 2) . Furthermore, the drug was more evenly distributed on the vessel surface compared to a DES (Figure 3) , . However, the effect was markedly lower when a solvent was used without the excipient iopromide. Therefore, a proper solubilising agent is important and excipients such as iopromide or urea are mandatory in balloon-based local drug delivery .
Early prototypes of coated balloon catheters, ca. 2001. Right: Paccocath balloon catheter before sterilisation. Clinical trial sample for the Paccocath ISR trial, 2003. Adapted from .
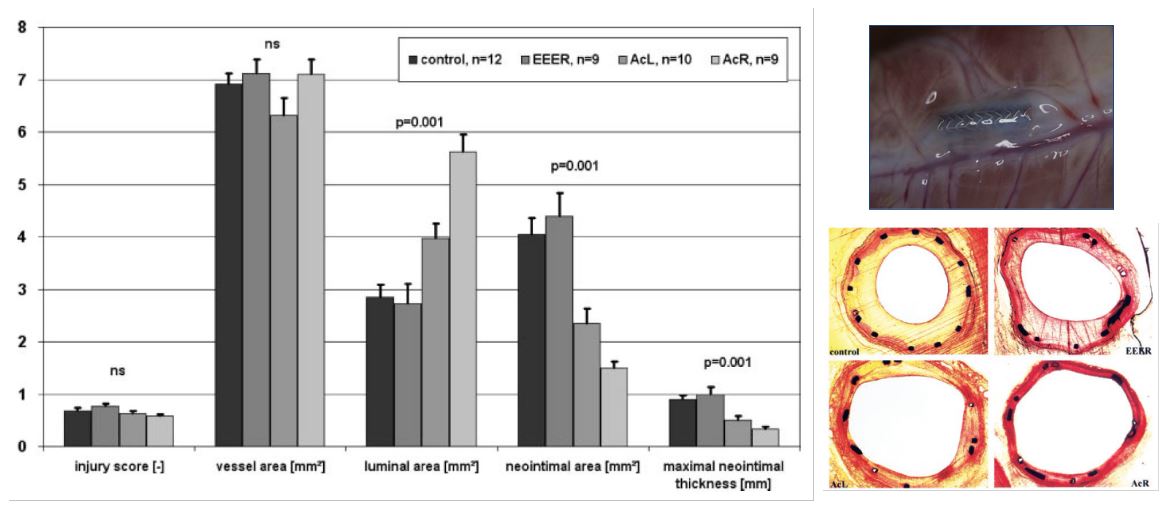
Histology and histomorphometry of stented porcine coronary arteries after 35 days. Implantation of bare metal stents with conventional PTCA catheters (control) and paclitaxel-coated, PTCA catheters with EEER coating or Ac coating (AcL and AcR). Parameters shown are injury score, vessel area, luminal area, neointimal area, and maximal neointimal thickness. Abbreviations are as defined in text. Values are mean±SD, n=40. EEER=ethyl acetate as the solvent with ≈2 μg paclitaxel/mm2 balloon surface, AcL=acetone as solvent with 1.3 μg paclitaxel/mm2 balloon surface (low dose paclitaxel), AcR=acetone as solvent with 2.5 μg paclitaxel/mm2 balloon surface (regular dose). Adapted from .
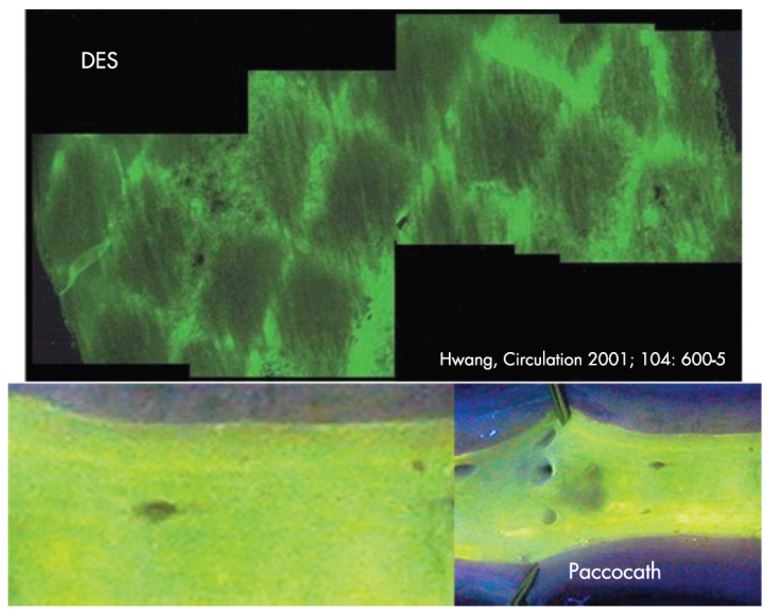
Inhomogeneous drug distribution from the luminal surface after stent implantation versus homogenous drug distribution from drug-coated balloon surface. Adapted from , .
It was shown that the balloon inflation time was not critical in the non-atherosclerotic porcine coronary stent model, e.g., treatment lasting 10 seconds reduced the neointimal area to the same extent as contact with the vessel wall for 2 times 60 seconds (by 57% and 56%, respectively, compared with control). These results suggest that balloons coated with a paclitaxel-matrix formulation release most of the drug rapidly during the first seconds of inflation . In addition, persistence of detectable drug in the vessel has been demonstrated to at least 6 months (Figure 4) .
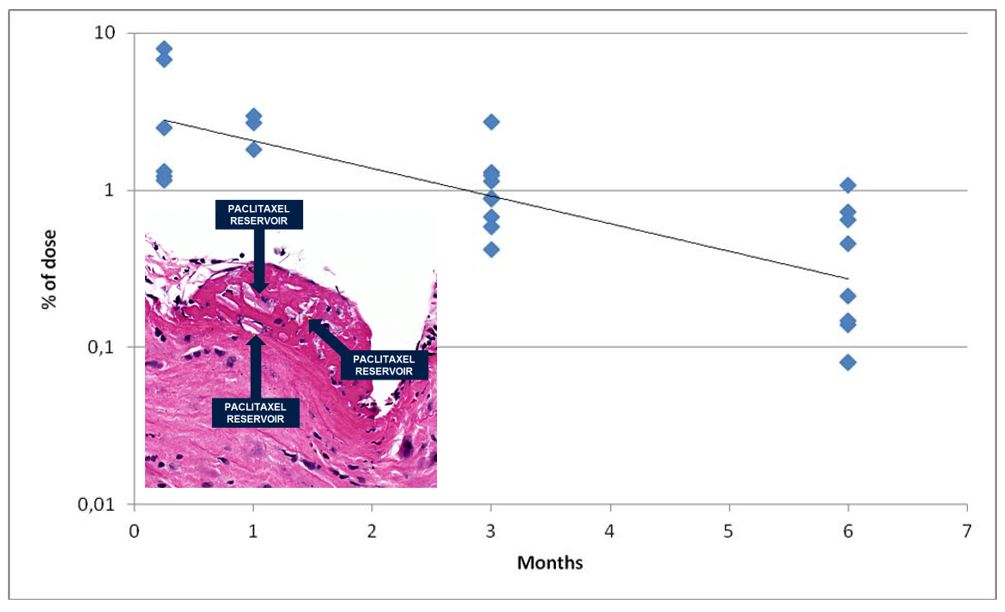
Paclitaxel content of porcine coronary arteries after a single treatment with an urea-based paclitaxel-coated balloon; half-life 1.7 months. Adapted from .
Since this initial research was published, several manufacturers have started commercialising or developing DCBs. Currently, paclitaxel is still the drug of choice, the typical dosage being 2 – 3.5 μg/mm2 of balloon surface. The critical factor enabling successful drug transfer is the formulation used to coat the balloon , , .
Coronary in-stent restenosis (ISR) is defined as a significant reduction (≥50%) in the luminal diameter within a previously stented segment or within the stent edges 5 mm proximal and distal to the stent . ISR can occur due to several pathophysiological mechanisms like elastic recoil, vascular smooth muscle cell proliferation, fibrin deposition and inflammatory response leading to neointimal hyperplasia and neoatherosclerosis . Technical factors associated with ISR include stent underexpansion or undersizing, vessel calcification, stent fracture, and geographic miss . Prior to the introduction of stents, plain balloon angioplasty (PBA) was associated with a 6-month restenosis incidence up to 60%, mainly due to acute elastic recoil and vessel remodelling . The introduction of bare metal stents (BMS) resulted in more predictable outcomes and less restenosis. However, the 1-year incidence of ISR remained around 20-30%, mainly due to excessive neointimal proliferation 3 to 6 months after BMS implantation. Drug-eluting stents (DES), by integrating a metallic stent platform with the release of an antiproliferative drug, have significantly reduced ISR with a 1-year incidence ranging from 2% to approximately 10%, depending on the individual risk profile and complexity of coronary artery disease . In up to 10% of all PCI procedures in the United States and approximately 5% of all PCI procedures in Europe, ISR continues to be the primary cause for percutaneous coronary re-intervention despite technical improvements in stent design. ISR is not benign, generates significant health care costs and is associated with an increased risk of death and rehospitalisation . In two small reports of patients with DES restenosis, 27% and 50% presented with a diagnosis of unstable angina pectoris and 5% and 11% presented with myocardial infarction . The treatment of ISR is challenging due to the extremely heterogeneous spectrum of underlying mechanisms. DES implantation and DCB angioplasty have been shown to be the most effective strategies in terms of both angiographic and clinical outcomes , leading to the current European Society of Cardiology guidelines recommending their prioritised use for the treatment of ISR (Class I) .
DES for the treatment of ISR is currently one of the most widely used therapeutic strategies. The superiority of DES implantation over several other therapeutic modalities for ISR has been demonstrated in head-to-head trials. In the DAEDALUS study, an individual patient meta-analysis including all 10 available randomised clinical trials comparing DCB angioplasty with DES implantation for treating ISR, patients allocated to DES showed a 3-year target lesion revascularisation rate of 12.0% . The randomised RESTENT-ISR trial showed no significant difference in the rate of major adverse cardiovascular events between everolimus-based and zotarolimus-based DES at 3 years (15.8% vs. 22.6%, p=0.276) . The randomised trial of ISR using a thin-strut bioresorbable DES (BIOLUX RCT) showed results similar to those of studies using DES with thicker struts and durable polymers . However, repeat stenting with DES also implies an additional permanent metallic layer that may replicate and promote the mechanisms leading to ISR, primarily neointimal hyperplasia and neoatherosclerosis. Although the antiproliferative drugs eluted after DES implantation for de novo coronary artery disease have been associated with reduced neointimal hyperplasia and ISR compared with BMS, the rates of early recurrent ISR after repeat stenting with DES for ISR are higher than those observed after treatment of de novo lesions . In addition, late ischaemic adverse events after DES implantation for ISR have sometimes shown an excess of late events compared with less effective treatments. These unanswered questions about the long-term safety of repeat DES implantation for ISR warrant more data with more modern devices.
One of the main advantages of a DCB-based approach is the elimination of an additional metallic layer that may further increase neointimal hyperplasia and neoatherosclerosis. In an early Japanese single-centre trial of 50 patients, DCB was associated with reduced angiographic late luminal loss (0.18±0.45 mm vs. 0.72±0.55 mm, p=0.001), which was reflected in reduced target lesion revascularisation rates (8.7±0.5% vs. 62.5%, p=0.0001) . The larger PEPCAD-DES (Treatment of DES-ISR With SeQuent Please Paclitaxel Eluting PTCA Catheter) trial confirmed in 110 patients with any type of DES-ISR that DCB angioplasty is significantly more effective than plain balloon angioplasty in terms of both late lumen loss (0.43±0.61 vs. 1.03±0.77; p<0.001) and target lesion revascularisation (15.3% vs. 36.8%; p=0.005) . The ISAR-DESIRE 3 trial, in which 402 patients with any -limus DES-ISR were randomly assigned in a 1:1:1 ratio to receive either balloon angioplasty, DCB angioplasty or repeat DES implantation, concluded that DCB was non-inferior to DES (p non inferiority=0.007) for in-segment percentage diameter stenosis . Both devices were superior to PBA (plain balloon, 54.1±25.0% vs. DCB, 37.4±21.8% vs. DES, 38.0±21.5%, p<0.0001 for DCB and DES vs. plain balloon). Incidences of target lesion revascularisation (TLR) at 1 year across plain balloon, DCB, and DES groups were consistent with angiographic follow-up at 6-8 months (PBA 43.5% vs. DCB 22.1% vs. DES 13.5%, p<0.0001 for DCB and DES vs. PBA) . At 3-year follow-up no significant differences in TLR were observed . In a subanalysis, no significant difference in post-procedure troponin levels among plain balloon, DCB, and DES was observed . Results from the final 10-year analysis of ISAR-DESIRE 3 demonstrated that the composite endpoint of all-cause death, myocardial infarction, target lesion thrombosis or target lesion revascularisation was significantly lower in the DCB and DES groups than in the PBA group (PBA 72.0% vs. DCB 55.9% vs. DES 62.4%, p<0.001) . This was mainly driven by lower incidence of TLR, while no significant difference was observed between DCB and DES (multiplicity-adjusted p=0.610; weighted Cox hazard ratio [HR] 1.10, 95% confidence interval [CI]: 0.80-1.51; Cox HR 1.10, 95% CI: 0.79-1.52; Royston-Parmar HR 1.08, 95% CI: 0.72-1.62). Target lesion revascularisation was significantly lower in the DCB and DES groups compared with the PBA group (PBA 58.0% vs. DCB 43.9% vs. DES 38.6%, p<0.0001), without a significant difference between DCB and DES (multiplicity-adjusted p=0.282) . In the landmark analyses, death and cardiac death were significantly more frequent in the DES group than in the DCB group within the first 5 years after percutaneous coronary intervention (death, multiplicatively adjusted p=0.028 and cardiac death, multiplicatively adjusted p=0.047) . Similar results were observed in a randomised clinical study conducted in China comparing paclitaxel DCB with paclitaxel DES in 220 patients with DES-ISR. DCB and DES were associated with comparable 9-month late lumen loss (0.46±0.51 vs. 0.55±0.61; p=0.32) and 2-year target lesion revascularisation (15.9% vs. 13.7%; p=0.66). DES were associated with an increased rate of death or MI compared with DCBs (3.7% vs. 11.8%, p=0.03), although the study was underpowered to evaluate clinical outcomes . The RIBS IV study showed that at 9 months after PCI, DES had a significant angiographic advantage over DCBs in terms of a significantly larger luminal diameter (2.03±0.7 mm vs 1.80.±0.6 mm, p<0.001) and a lower percentage of diameter narrowing (23%±22% vs. 30%±22%, p<0.01) . At one year, the primary composite endpoint of cardiac death, myocardial infarction or target vessel revascularisation was significantly lower in patients allocated to DES compared to those allocated to DCB (10% vs. 18%; HR 0.58, 95% CI: 0.35-0.98; p=0.04), mainly due to a significant reduction in target vessel revascularisation (8% vs. 16%; p=0.035) .
Recent results from AGENT IDE, the US pivotal randomised trial of DCB for the treatment of DES-ISR, demonstrated the superior clinical efficacy of DCB compared to balloon angioplasty in reducing the rate of the composite endpoint of target lesion failure, defined as the composite of cardiac death, target vessel myocardial infarction or ischaemia-driven target lesion revascularisation (17.9% vs. 28.6%; HR 0.59, 95% CI: 0.42-0.84; p=0.003) . At one-year TLR (13% vs. 24.7%; HR 0.50, 95% CI: 0.34-0.74; p=0.001) and target vessel MI (5.8% vs. 11.1%; HR 0.51, 95% CI: 0.28-0.92; p=0.02) were significantly lower with DCB compared with plain balloon. The results from the AGENT IDE study have recently resulted in the first coronary DCB being approved in the US.
The preparation of lesions is of pivotal importance in the treatment of ISR, particularly when treated by DCB angioplasty. Consequently, it is recommended that the entire lesion length should be treated using gradual predilation with plain balloons of increasing size, resulting in a residual stenosis of less than 30% without significant dissection (≥type C) or impairment of coronary flow (Thrombolysis in Myocardial Infarction [TIMI] <3). This approach is considered to be beneficial for DCB angioplasty. Among 166 ISR lesions treated with DCB, the cumulative TLR rate was significantly lower (20.3% vs. 35.5% at 2 years; p=0.04) when lesion preparation fulfilled the DCB consensus criteria . The difference was even more pronounced in a study including 256 patients (309 lesions). After 2 years, TLR was only 8.3% if residual stenosis <20% was achieved by lesion preparation . The DCB diameter was at least 91% of the stent and the inflation time was >60 seconds. After only partial compliance with these quality parameters, the TLR rate had already more than doubled (19.2%).
Some devices that have demonstrated limited efficacy when utilised as a standalone treatment for ISR, such as cutting or scoring balloons, have been shown to enhance the success of revascularisation when integrated into combined strategies , . There is a growing interest in traditional and novel debulking devices, such as rotational atherectomy and intravascular lithotripsy, for the treatment of ISR prior to DCB angioplasty.
In early randomised trials, rotational atherectomy followed by plain balloon angioplasty for the treatment of ISR did not result in significant angiographic or clinical benefits compared with standalone plain balloon angioplasty . Nevertheless, it may be reasonably considered that adjuvant rotational atherectomy before DCB angioplasty or DES implantation for the treatment of diffuse, severely obstructive, and recurrent ISR may be a viable option.
Intravascular lithotripsy is a recently introduced technique based on the locoregional emission of shock waves by multiple emitters positioned in heavily calcified lesions. Once the target lesion is reached, the balloon is inflated at low atmospheric pressure, and one or more cycles of sonic waves are delivered to fragment the calcified plaque mass. There are currently no randomised trials in the setting of in-stent restenosis (ISR). However, several case reports have demonstrated the feasibility of this technique for ISR as a potential therapeutic option for calcium debulking .
(Figure 5) illustrates the proposed algorithm for the treatment of in-stent restenosis with a primary drug-coated balloon strategy .
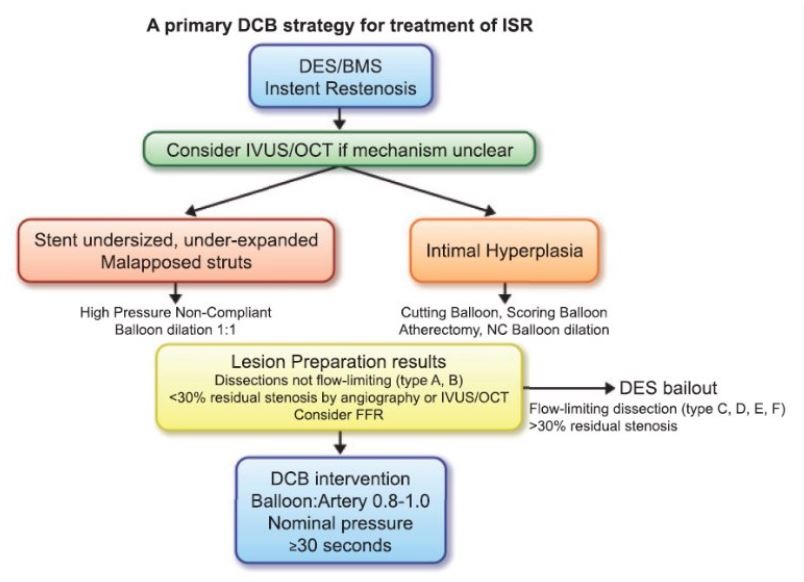
Proposed algorithm for the treatment of in-stent restenosis with a primary drug-coated balloon strategy. Adapted from (48).
Current guidelines do not recommend DCB for the treatment of de novo coronary lesions . For most interventional cardiologists, it is still difficult to imagine treating a lesion without a stent. The argument against DCB is usually based on the allegedly high number of acute vascular occlusions. A propensity-matched cohort from the SCAAR registry including 1,197 DCB and 1,197 current-generation DES showed a significantly lower rate of target lesion thrombosis after DCB-only treatment with a hazard ratio of 0.18 (0.2 vs. 1.1%) . In BASKET-SMALL 2, no acute vessel closure occured in DCB-only treated lesions . The basic prerequisite, however, is the identification of lesions at risk. This is achieved by careful preparation of the lesion . The main advantages of DCB therapy become apparent in de novo lesions. The use of a DCB allows the number and length of stents to be reduced . Together with dual platelet therapy, this DCB-only concept has proven to be safe in many registries and randomised trials . However, it should be noted that the recommendations of the DCB consensus group on lesion preparation and its goals are predominantly expert opinions by operators with extensive DCB experience.
Coronary vasomotion is highly implicated in various stages of coronary artery disease. DCB angioplasty is expected to reduce the risk for adverse events related to permanent coronary implants, which is based on the assumption that the absence of metallic caging would facilitate restoration of vasomotion. Kim et al investigated 89 patients who received DCB-only treatment and an ergonovine provocation test at 6-9 months follow-up. The lesions treated with DCB were not particularly vulnerable to vasospasm and were found to have vasomotor function similar to angiographically normal segments . In a randomised fashion, Kawai et al compared coronary vasomotion in patients with small coronary artery disease treated with DCB versus DES. At eight months, vasoconstriction after acetylcholine infusion was less pronounced in the DCB arm than in the DES arm, suggesting that endothelial function in treated coronary vessels could be better preserved by DCB than by new-generation DES .
A unique result, found especially after paclitaxel DCB treatment, is late lumen enlargement , which means that a non-stent-like result can be accepted initially, and an improvement of the vessel lumen occurs over the course of a few months. One of the advantages of stent treatment is the prevention of elastic recoil and, consequently, superior primary lumen gain. However, such a permanent implant is associated with a loss of lumen over time. In contrast, after DCB treatment, a stent-like result can rarely be achieved. We have demonstrated that de novo coronary lesions treated with ‘DCB-only’ show late lumen enlargement (LLE) after four months with a rightward shift of the minimal lumen diameter (MLD) distribution curve. LLE has been observed in about 60% of all patients . This benefit also applies to the ostium of side branches , in the setting of bifurcation lesions. While this induces a theoretical risk of coronary artery aneurysm formation, no excessive rate has been reported after DCB angioplasty .
The pathomechanism of LLE has been described by intravascular ultrasound measurements as the enlargement of the total vessel area followed by an increase of the vessel’s lumen , . This finding is very similar to the compensatory vessel enlargement in the early phase of atherosclerosis which may be explained by an accumulation of paclitaxel in the adventitia . In a case report, we were able to show for the first time that after DCB-only treatment, the atherosclerotic plaque burden was significantly lower than in the untreated and, according to angiographic criteria, healthy areas . Recent experimental findings show an inhibition of local inflammation and lesion progression in experimental atherosclerosis in rabbits . In a large series, Yamamoto et al reported a reduction in plaque volume, implying a regression of atherosclerosis .
The old axiom "the more you gain, the more you lose" applies to balloon angioplasty, as greater primary lumen gain is accompanied by an increase in lumen loss . For angioplasty with DCB, on the other hand, the occurrence of dissections seems to be helpful. In the THUNDER trial on femoropopliteal lesions, the uncoated balloon group had a marked difference in late lumen loss (LLL) between grade A/B dissections and grade C/D/E dissections. After uncoated balloon angioplasty, severe dissections resulted in an increase in LLL. In contrast, in the DCB group, lesions with severe dissection (grades C, D or E) benefited more from treatment with a coated balloon . The use of intravascular ultrasound (IVUS) in femoropopliteal disease improves acute gain and is associated with a reduction of LLL when using paclitaxel-coated DCB , .
ULTIMATE III was a randomised trial that compared IVUS-guided with angiography-guided DCB-only PCI in patients with de novo lesions and high bleeding risk . The final results at 7 months demonstrated that IVUS-guided PCI was associated with less late lumen loss compared with angiography-guided PCI. A possible explanation for these results is better lesion preparation as the IVUS-guided group used approximately 0.25 mm larger balloons than in the angiography-guided group. The results of the TRANSFORM I study, where a reduction in angiographic late luminal loss was found for the paclitaxel-coated DCB with an increasing dissection volume, also fit in with this , . Whether these results could translate to better patient outcomes remains to be seen as this trial was not powered for clinical outcomes.
These findings call the old doctrine of gain associated with loss into question. This means that, at least for clinically proven paclitaxel coatings, the old axiom no longer stands and is now simply "the more you gain, the more you get" when using paclitaxel-coated DCB (Figure 6) .
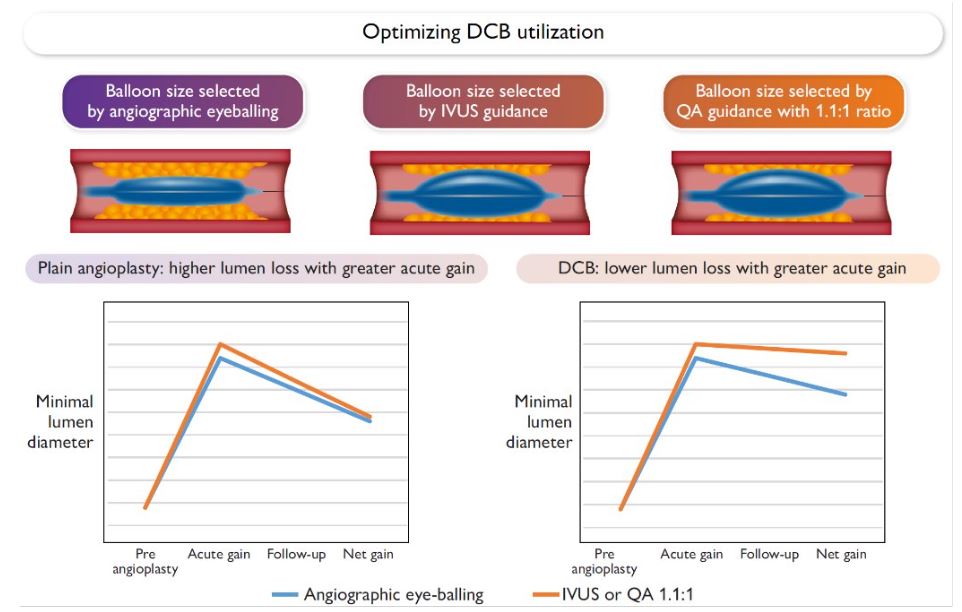
The more you gain the more you get. Benefits of an aggressive primary treatment of femoropopliteal artery disease guided by intravascular ultrasound (IVUS) or quantitative angiography (QA) with balloon oversizing of 1.1:1. Proposed mechanisms of an improved initial lumen gain resulting in reduced net gain at follow-up after uncoated angioplasty (left) or the additional effect of higher dissection grade on late lumen loss after paclitaxel-coated balloon (DCB) treatment (right). Adapted from (73).
The main principle of balloon angioplasty is to achieve lumen gain in a stenotic segment of an epicardial vessel. Balloon inflation and its associated barotrauma leads initially to compression of the plaque. However, simple plaque compression in most cases will not lead to lumen enlargement . Plaque rupture with vessel dissection usually caused by overstretching of the vessel has been identified as the main mechanism of lumen gain , . Angiographically visible dissections are present in about 20-40 % of PTCA procedures and about 5% can be associated with acute vessel closure. Therefore, appropriate identification of the dissection type is crucial to guiding further treatment . It has been shown that non-flow-limiting dissection types A and B, classified according to the National Heart, Lung, and Blood Institute’s system, with no further treatment (left to heal spontaneously), are not associated with increased morbidity and mortality . In particular, this has been demonstrated after treatment with DCB . In turn, dissections classified as types C through F, which are in most cases accompanied by impaired coronary flow, are strongly associated with poor short- and long-term outcomes . Therefore, the latter dissections should be treated more aggressively in order to re-establish normal coronary flow and to prevent further spread. This usually involves scaffolding of the vessel with drug-eluting stents. However, a hybrid approach with implantation of DES at the proximal and/or distal end of the dissection and DCB between the stents or in distal parts of the dissections (when DES is placed proximal) may be a reasonable option.
Barotrauma applied to the vessel aiming to disrupt the plaque leads to disruption of the tunica intima (endothelium) and, to some extent, media as well. This triggers platelet activation and their adhesion as a part of a normal response to the vessel injury. Furthermore, injury promotes proliferation of smooth muscle cells and enhances fibrocellular proliferation. These processes have been termed intimal hyperplasia and have been associated with restenosis (defined as a stenosis grade >50% in the treated lesion). Early evidence has suggested that neointimal hyperplasia is the key mechanism of restenosis , . However, it is more probable that restenosis is in fact multifactorial . Data from imaging studies have suggested that the key mechanism of restenosis is negative vessel remodelling, contrary to neointimal hyperplasia .
Vulnerable plaque (VP) as a term and a concept has increasingly attracted the attention of interventional cardiologists due to the growing body of evidence that timely detection and treatment can influence patient outcomes (81-83). Several features of VP have been postulated, such as the presence of thin-cap fibroatheromas (TCFA), characterised by a large necrotic core rich in foamy macrophages covered by a thin cap of fibrous tissue (≤65 µm) , . In the majority of cases, these VP are not associated with the relevant narrowing of the coronary vessel, and therefore do not cause ischaemia on exertion , . However, they have been recognised as a substrate associated with acute coronary syndrome (ACS) and sudden cardiac death through the acute onset of ischaemia due to thrombosis , . Three key lesion types are plaque rupture, plaque erosion and calcific nodules. The most common is plaque rupture which is more common in men, followed by plaque erosion which is especially common in young women (<50 years of age) . Using intravascular imaging, the high-risk features of VP have been further identified: i) based on virtual histology intravascular ultrasound (VH-IVUS), a minimum lumen area (MLA) ≤4 mm2, plaque burden ≥70% or a TCFA phenotype , ; ii) based on optical coherence tomography (OCT): an MLA of <3.5 mm2, a fibrous cap thickness of <75 µm, a lipid arc of >180°, or macrophages ; iii) based on near-infrared spectroscopy (NIRS)-IVUS, plaque burden ≥70% and a lipid-rich plaque (maxLCBI4mm >325) , . The use of cardiac computed tomography angiography (CCTA) has also been suggested as a way to identify high-risk atherosclerotic plaque with the following features: positive remodelling, low-attenuation plaque, spotty calcification and a napkin-ring sign .
According to one retrospective analysis in patients with ACS caused by vulnerable plaque confirmed using IVUS, treatment with DCB compared with DES showed comparable results in term of incidence of major adverse cardiovascular events (MACE) and restenosis. Moreover, the diameter of LLL was smaller in the DCB group than in the DES group .
The recently published DEBuT-LRP study included patients presenting with non-ST-segment elevation acute coronary syndrome (NSTEMI). Lesions with a maximum lipid core burden index (imaxLCBI) ≥325 underwent additional paclitaxel DCB treatment. The pre-emptive treatment of non-flow-limiting, non-culprit vulnerable lipid-rich plaques with a paclitaxel-coated balloon resulted in a significant reduction of the lipid burden (maxLCBI4mm) without overt safety concerns .
One of the basic prerequisites and also the key point for reaching a good long-term result in treatment with DCB is appropriate lesion preparation (Figure 7) . In proper lesion preparation, predilatation normally starts with semi-compliant (SC) balloon angioplasty, the appropriately sized balloon should be selected with a balloon-to-vessel ratio of 1.0-1.0 based on distal reference vessel diameter (RVD). For this purpose, pressure between 8-10 bar should be applied to reach the nominal diameter as a higher applied pressure may not result in equally applied force. In case of inadequate balloon expansion or the presence of a ‘‘dog-bone’’ effect due to calcified lesions or remaining relevant stenosis, either a non-compliant (NC) balloon or scoring and cutting balloons may be reasonable options . Applying higher pressure using an NC balloon (up to 25 bar) leads to a more equalised inflation without a relevant increase above the nominal diameter. The high pressure creates a greater radial force which is applied to the lesion. Furthermore, use of NC, or cutting and scoring balloons should be strongly considered in order to prevent the so called “watermelon seeding’’ phenomenon, which may lead to displacement of the guide catheter which could lead to dissection of the ostial parts of the major coronary vessels . As a rule, ostial lesions, especially those with poor blood flow (< TIMI III) should be promptly scaffolded using DES. This could be especially challenging when these dissections occur in the area of the left main with a potentially fatal outcome due to a rapid onset of haemodynamic instability.
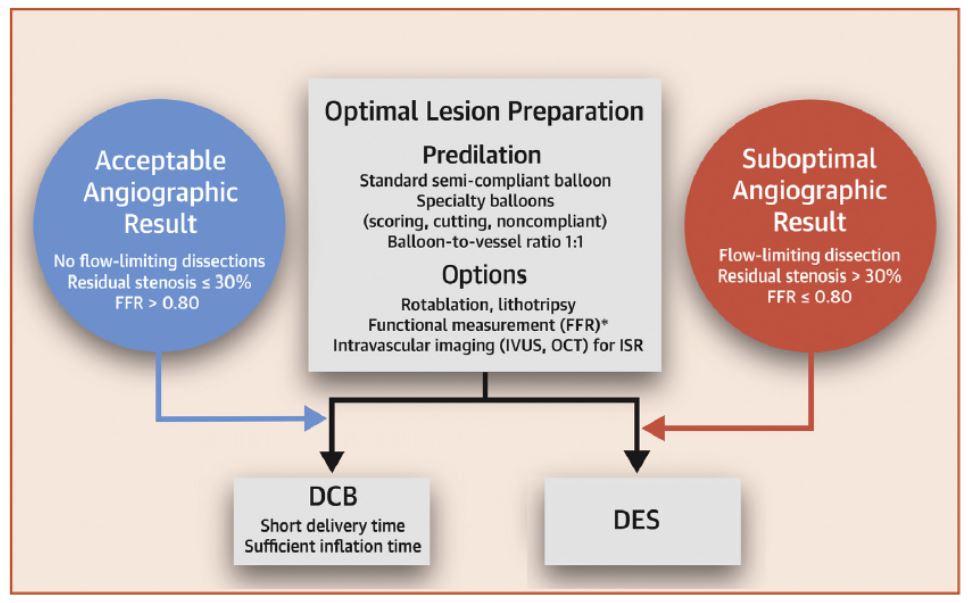
General algorithm for treatment of de novo lesions according to the international DCB consensus group. Focus on lesion preparation, decision between DCB or DES depending on the result of lesion preparation. Adapted from .
According to the results of the ISAR-DESIRE 4 trial, neointimal modifications using scoring balloons prior to the final treatment of in-stent restenosis with a DCB, lead to better long-term results with less frequent in-segment stenosis and late lumen loss, while having comparable safety issues (death or myocardial infarction) . Therefore, it is highly recommended to use scoring balloons regardless of whether they are used following primary angioplasty with an SC balloon or for primary angioplasty alone.
A retrospective analysis of 259 patients (278 lesions) treated with DCB for de novo lesions showed a higher prevalence of residual diameter stenosis ≤ 30%, when using scoring balloons (68.9% vs. 39.6%, p<0.001), while severe dissection, defined as type C or greater, was observed less frequently (9.8% vs. 31.8%, p=0.001). Moreover, the scoring balloon group achieved a superior rate of optimal angiographic results (60.7% vs. 28.6%, p<0.001) . Figure 8 presents an example of stepwise lesion preparation including scoring balloons.
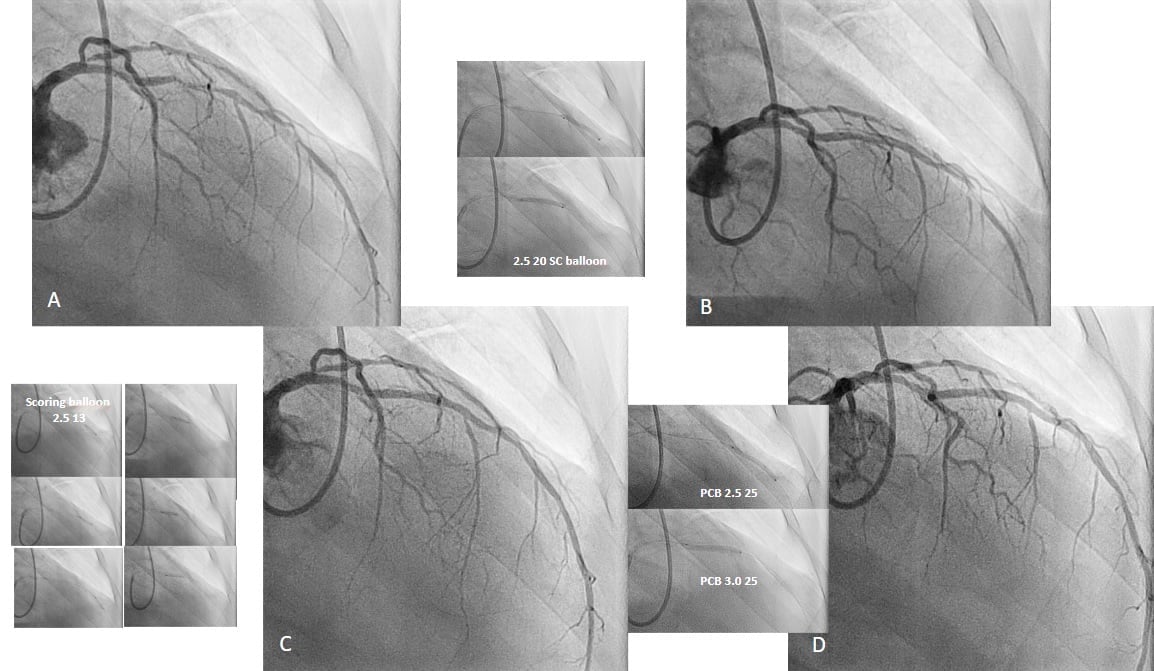
Example of stepwise lesion preparation in a 68-year-old male presenting with diabetes, hypertension, ex-smoker, angina CCS III. A) Long diffuse disease in the mid-left anterior descending artery. B) Dissection and insufficient lumen gain in the distal part after semi-compliant balloon inflation. C) Reduced dissection grade and improved lumen gain in the whole segment after multiple scoring balloon inflations. D) Final result after 2 paclitaxel DCB.
However, in severely calcified lesions, the use of scoring-, cutting- or an NC-balloon will not lead to adequate lesion preparation. These lesions are recognised as the angiographic occurrence of radiopacities in the absence of cardiac motion and contrast injection that affects both sides of the arterial wall (so called “tram-track” appearance) . These kinds of lesions are present in about 20% and are associated with poor procedural success and poor long-term outcome , . The use of intravascular imaging here is crucial and highly recommended in order to gain additional information concerning the severity of the calcification (depth, length, thickness) and its morphology (concentric, eccentric, nodular, microcalcification) both of which are pivotal for further treatment strategy , .
In severely calcified lesions with characteristics such as calcium arch > 180°, calcium length >5 mm, and/or calcium thickness >0.5 mm, some of the available calcium debulking strategies such as rotational/orbital atherectomy and intravascular lithotripsy should be strongly considered to help achieve optimal lesion preparation. Balloon crossable lesions with deep calcium (located at >50% of the depth of the plaque) should be treated using intravascular lithotripsy. Balloon non-crossable lesions should be treated with rotational or orbital atherectomy .
Data from retrospective registries have suggested the feasibility of rotational atherectomy and orbital atherectomy in severely calcified lesions prior to DCB treatment, while these kind of data to the best of our knowledge are not available for intravascular lithotripsy.
For an optimal result after initial lesion preparation, the final treatment ends with inflation of the DCB over a period of 30-60s. An acceptable angiographic result after lesion preparation is defined according to the 3rd report of the international DCB consensus group as follows: i) the balloon used for angioplasty should be fully inflated; ii) residual stenosis assessed visually should not exceed 30%; iii) TIMI flow grade 3; iv) no presence of flow-limiting dissections (type C-F) .
If the angiographic findings are unclear, in regard to stenosis grade or uncertainty regarding the remaining type of dissections (delayed contrast clearing), fractional flow reserve (FFR) or intravascular imaging (IVUS or OCT) should be considered for further clarification. Indeed, data from the REDUCE-STENT retrospective registry are reassuring in terms of safety after final treatment with DCB in case of an imperfect angiographic result after lesion preparation, when the distal coronary-to-aortic pressure ratio (Pd/Pa) is >0.90 . This registry included 86 patients with 109 lesions in total. After comprehensive lesion preparation utilising cutting balloons (25.7%), rotational atherectomy (6.4%) and intravascular lithotripsy (9.2%), 79 (72.5%) lesions with Pd/Pa >0.90 were treated with DCB-only. In 6 lesions with Pd/Pa <0.90, DES were used, and in 14 lesions with Pd/Pa <0.90 a hybrid approach using DES for proximal parts of the vessel and DCB for distal ones were used. There were no cases of acute vessel occlusion. Of note, in patients with ST-elevation myocardial infarction (STEMI) in acute settings, the use of FFR was not reliable for assessing the haemodynamic relevance of residual stenosis in culprit lesions because of microvascular dysfunction . Still, FFR-guided revascularisation of non-culprit lesions in patients with STEMI reduced repeat revascularisations in comparison with angiography-guided PCI during the index procedure in patients with multivessel disease . In patients with NSTEMI, it seems that FFR-guided PCI is safe and accurate for both culprit and non-culprit lesions .
It has been shown that intravascular imaging (IVUS or OCT) -guided PCI compared with angiography alone-guided PCI is associated with better patient outcome in terms of a reduction of the composite endpoint of cardiac death, target vessel-related myocardial infarction or clinically driven target vessel revascularisation in patients with complex coronary lesions and complex bifurcation lesions . The use of intravascular imaging may overcome some of the weaknesses of angiography alone-guided PCI, and facilitate the identification of culprit lesions among patients with ACS , , as well as aid in selecting the appropriate DES size to avoid underexpansion and malapposition (presence of a gap between an implanted DES and the intima of the vessel) after PCI when DES have been used as a final treatment. However, the evidence supporting intracoronary imaging is based on the fact that PCI uses stent implantation. There are some retrospective data about OCT-guided DCB treatment in patients with ACS . During the median follow-up period of 562 days, 24 patients (18.9%) suffered target lesion failure (TLF; defined as composite of cardiac death, target vessel-related myocardial infarction and ischaemia-driven target lesion revascularisation) and 103 (81.1%) did not. Based on OCT-driven data, factors like plaque morphology and residual thrombus burden have been strongly associated with TLF .
The totality of the evidence on intravascular imaging (IVUS or OCT) provides no clearly defined criteria to guide physicians on when to use DCB instead of DES and vice versa once lesion preparation has been performed. Furthermore, imaging findings immediately after primary angioplasty may sometimes be discouraging and for interventional cardiologists without sufficient expertise in treatment with DCB, can be, in fact, misleading. For example, the presence of microthrombi and no flow-limiting dissections in combination with some extent of vasospasm may result in a small minimal lumen area (MLA) of less than 3.5 mm2, a cut-off value that has been associated with worse long-term outcomes . This could be further misinterpreted as inadequate lesion preparation which may then lead to more aggressive lesion preparation, thus increasing the risk for occurrence of hazardous dissections type C-F. In line with this, there are data that suggest that treatment with DCB is associated with positive vessel remodelling such as late lumen enlargement . Therefore, data from trials that assessed the use of intravascular imaging after use of DES cannot be translated into a ‘stent-free’ DCB strategy. In a real world scenario, this would mean that intravascular imaging should be used in case of uncertainty but in some cases a suboptimal result like those with MLA <3.5mm2 accompanied with a good TIMI 3 flow may be accepted as a final result and checked using a non-invasive (exercise echocardiography, cardiac-CT scan) or invasive (angiography) approach at a later follow-up (1-3 months after index PCI).
The management of obstructive disease of small coronary vessels remains a particularly challenging issue in routine clinical practice. The inverse correlation between vessel calibre and antirestenotic efficacy after percutaneous intervention is well-documented . Early investigations demonstrated that bare metal stent (BMS) implantation in vessel segments with a smaller diameter was associated with a markedly elevated incidence of ISR at angiographic follow-up . Although the introduction of DES has reduced the incidence of TLR in small vessels, this anatomical subset continues to present technical difficulties and inferior outcomes. In the context of the aforementioned circumstances, DCB angioplasty for small-vessel disease (SVD) represents a compelling treatment option that may potentially reduce both restenosis and target lesion thrombosis by circumventing the implantation of a permanent metallic layer. The preliminary findings from the prospective, single-arm PEPCAD study indicated that the use of an angioplasty balloon catheter with a paclitaxel iopromide coating for the percutaneous treatment of coronary artery disease was associated with a favourable safety and efficacy profile at 12-month follow-up . Among patients who did not require the use of a bailout stent with a BMS, the incidence of cardiac death, target vessel myocardial infarction, or TLR at 12 months was 6.1%. It is noteworthy that these favourable results remained unchanged at 36 months, with no additional target lesion-related events occurring after 12 months.
The pivotal BELLO (Balloon Elution and Late Loss Optimization) trial included a total of 182 patients with SVD, randomly assigned to DCB angioplasty or paclitaxel DES implantation . At 6-month angiographic follow-up, DCB not only demonstrated non-inferiority but also superiority to DES in terms of the primary endpoint of late lumen loss (0.08±0.38 mm vs. 0.29±0.44 mm; p non-inferiority<0.001; p superiority=0.001). However, the trial was designed to prove only non-inferiority and rates of bailout BMS implantation were as high as 20%. It is of interest to note that at 12 months, no safety concerns related to DCB technology were observed . The subsequent 24-month analysis demonstrated that the cumulative incidence of all-cause death, myocardial infarction, or target vessel revascularisation was significantly lower in the DCB group (14.4% vs. 30.4%, p=0.015) . At 36 months, the Kaplan-Meier method showed a statistically significant difference in MACE between the groups (DCB 14.4% vs. PES 30.4%) . In the same period, a small randomised clinical trial comparing 135 patients with small vessel disease assigned to DCB angioplasty or plain balloon angioplasty in a 2:1 ratio was conducted. At 6-month angiographic follow-up, DCB angioplasty was associated with a lower late lumen loss compared with plain balloon angioplasty (0.01±0.31 vs. 0.32±0.34 mm). There was also a numerical trend towards a reduced incidence of target lesion revascularisation with DCB (3.4% vs. 10.3%), but the difference was not statistically significant .
In the BASKET-SMALL 2 trial, 758 patients were randomly assigned to DCB angioplasty or DES following adequate lesion preparation (residual stenosis ≤30%, Thrombolysis in Myocardial Infarction (TIMI) 3 flow grade, and National Heart, Lung, and Blood Institute dissection grade ≤B) . The trial was designed to assess the non-inferiority of DCB in terms of a composite endpoint of major adverse cardiac events, including cardiac death, non-fatal myocardial infarction, or target vessel revascularisation, at 12 months in the per-protocol cohort. A total of 14% of patients diagnosed with de novo stenosis were not eligible for inclusion due to suboptimal angiographic results following predilation. About 25% of patients received paclitaxel DES, and the remaining patients received a second-generation everolimus-DES. At 12 months, DCB angioplasty was non-inferior to DES implantation in the per-protocol cohort (p non-inferiority=0.022). The incidence of the individual endpoints of cardiac death (3.1% vs. 1.3%; HR 2.33, 95% CI: 0.82-6.61), non-fatal myocardial infarction (1.6% vs. 3.5%; HR 0.46, 95% CI: 0.17-1.20), and target vessel revascularisation (3.4% vs. 4.5%; HR 0.75, 95% CI: 0.36-1.55) did not significantly differ between DCB angioplasty and DES implantation . The three-year follow-up results demonstrated that both DCB and DES were associated with an incidence of cardiac death, non-fatal myocardial infarction, and target-vessel revascularisation of 15% (HR 0·99, 95% CI: 0.68-.45) . The individual endpoints of cardiac death (5% vs. 4%; HR 1·29, 95% CI: 0.63-2.66), non-fatal myocardial infarction (6% vs. 6%, HR 0·82, 95% CI: 0.45-1.51), and target vessel revascularisation (9% vs. 9%; HR 0·95, 95% CI : 0.58-1.56) were not significantly different between groups.
The RESTORE Small Vessel Disease trial involved 230 patients presenting with de novo disease of small vessels who were randomised to either paclitaxel DCB or second-generation zotarolimus-DES . At 9-month angiographic follow-up, DCB angioplasty was shown to be non-inferior in terms of the primary endpoint of in-segment percentage diameter stenosis (29.6±2.0% vs. 24.1±2.0%, p non-inferiority<0.001) in comparison to DES implantation. The DCB cohort demonstrated a smaller in-segment minimum lumen diameter (1.40±0.42 mm vs. 1.71±0.39 mm; p<0.001) and comparable late lumen loss (0.25±0.42 mm vs. 0.27±0.36 mm; p=0.73) in comparison to the DES cohort. At 12 and 24 months, there were no differences between DCB and DES in cardiac death, target vessel myocardial infarction, or TLR (4.4% vs. 2.6%; p=0.73 and 5.2% vs. 3.7%; p=0.75, respectively) and in each individual component of the composite endpoint .
The PICCOLETO II (Drug Eluting Balloon Efficacy for Small Coronary Vessel Disease Treatment II) trial, showed that at a median angiographic follow-up of 189 days, a paclitaxel DCB was non-inferior and superior to a second-generation everolimus-DES in terms of the primary endpoint of in-lesion late lumen loss (0.04±0.28 mm vs. 0.17±0.39 mm; p non-inferiority=0.001; p superiority=0.03) . In-lesion binary restenosis (6.5% vs. 6.3%; p=0.98) and percent diameter stenosis (21.6±13% vs. 25.1±11%; p=0.37) were not significantly different between DCB and DES. At 12 months, the composite endpoint of cardiac death, myocardial infarction, or TLR (7.5% vs. 5.6%; p=0.51) were not significantly different between DCB and DES. The final follow-up of this study was recently published. After 3 years, the authors reported a significant reduction in abrupt vessel closure and MACE in the DCB arm (10.8% vs 20.8%; p=0.046) . In consideration of this, another recent meta-analysis has reported the results of DCB versus DES in de novo SVD, including five RCTs (1,459 patients; DCB n=734 and DES n=725) . Over a 6-month follow-up period, the authors found that DCB were associated with a lower level of late lumen loss (LLL) compared with DES (mean difference of –0.12 mm, p=0.01). Additionally, they observed that DCB were linked to a lower incidence of ISR and a similar incidence of major adverse cardiovascular events, cardiovascular mortality, TLR and target vessel revascularisation (TVR) compared with DES at 1 year.
Sánchez et al included five RCTs in their meta-analysis comparing DCB with DES with a mean clinical follow-up of 10.2 months . In this study, the use of DCB was found to be associated with a similar risk of TVR (odds ratio [OR] 0.97, 95% CI: 0.56-1.68; p=0.92), TLR (OR 1.74, 95% CI: 0.57-5.28; p=0.33), and all-cause death (OR 1.03, 95% CI: 0.14-7.48; p=0.98), with a significantly lower risk of vessel thrombosis (OR 0.12, 95% CI: 0.01-0.94; p=0.04).
The interpretation of differences in available evidence on DCBs for small-vessel disease is challenging and likely multifactorial. However, the above-mentioned study results and meta-analysis supports the use of DCB in small vessel diseases as an alternative to DES, when lesion preparation is sufficiently accomplished.
The growing evidence supporting the safety and efficacy of DCB in de novo large coronary arteries is leading to an increasing interest in the use of DCB alone or as part of a hybrid strategy in combination with DES, with the aim of avoiding long metallic implantations. A recent trial randomised 288 patients with lesions with a reference vessel diameter between 2.25 and 4.00 mm and lesion length ≤30 mm to the SeQuent Please DCB or a DES. The 9-month LLL was −0.19±0.49 mm in the DCB versus 0.03±0.64 mm in the DES arm (p=0.019), while 12-month MACE was similar (2.44% vs 6.33%; p=0.226) . In another smaller, multicentre, prospective, observational study enrolling 119 patients with de novo coronary lesions in vessels ≥2.75 mm in diameter, a DCB-only strategy also appeared to be safe and effective for both bifurcation and non-bifurcation lesions. Two-year follow-up revealed TLF, TLR, and TVR rates of 4.0%, 3.4%, and 4.2%, respectively .
In another study, using a propensity score matching analysis, the authors compared a SeQuent Please DCB to a new-generation DES for ostial lesions in the left anterior descending artery . At 12-month follow-up, the outcomes were similar between the two groups (MACE: 6% vs 6%; p=1.0; TLR: 2% vs 4%; p=0.56), suggesting the feasibility and safety of this stentless approach for ostial lesions of large vessels.
In the left main stem, Liu et al demonstrated that a hybrid strategy, which involved the use of a DCB in the secondary branch in addition to a DES in the main branch, was more effective than a two-stent strategy in terms of LLL . A statistically significant difference was observed in the minimum lumen diameter at the mid-segment (‒0.17 mm vs 0.43 mm; p<0.001) and at the proximal main branch (0.09 mm vs 0.17 mm; p=0.037). In a separate study, directional atherectomy was employed prior to DCB treatment of bifurcation lesions, with 80% of lesions located in the left main . A true bifurcation was present in only 14% of cases, thus indicating that DCB were primarily utilised in the main vessel (and in 3.9% of cases in the side branch). A 12-month follow-up demonstrated favourable procedural outcomes, with low rates of restenosis (2.3%) and TLR (3.1%), as well as an acceptable rate of target vessel failure (10.9%), driven only by TVR .
Despite the encouraging results of some smaller studies, there is a need for further, larger randomised clinical trials to be carried out in order to provide a more definitive answer as to whether DCB are a more appropriate option than DES in the treatment of large vessel disease.
It is estimated that up to 20% of percutaneous coronary interventions are complicated by coronary bifurcation disease. The management of bifurcation lesions continues to yield suboptimal results, particularly in the context of the side branch. This represents a significant area of investigation, particularly in the context of DCB, given its potential role in addressing this challenge .
Initial randomised clinical trials explored the combination of DCB plus BMS for the treatment of coronary bifurcation lesions with unfavourable results. In the DEBIUT (Drug-Eluting Balloon in Bifurcations) trial, 117 patients were 1:1:1 randomly assigned to DCB angioplasty of both branches followed by BMS implantation in the main vessel, BMS implantation in the main vessel and plain balloon angioplasty of the side branch, or paclitaxel DES implantation in the main vessel and plain balloon angioplasty of the side branch . Kissing balloon after provisional stenting was recommended regardless of the strategy assigned. At 6-month angiographic follow-up, the strategy based on DCB failed to show significant differences compared with the BMS-based strategy and was shown to be less effective than the DES-based strategy .
In the BABILON (Paclitaxel-Coated Balloon in Bifurcated Lesions) trial, a total of 108 patients were randomly assigned to undergo sequential predilation and DCB angioplasty of both branches, followed by provisional BMS implantation in the main branch, or sequential predilation of both branches, followed by provisional everolimus-DES implantation in the main branch . The DCB plus BMS strategy was found to be non-inferior to the DES-alone strategy in terms of in-segment late lumen loss after 9-month (0.31±0.48 vs. 0.16±0.38 mm, p non-inferiority=0-001, p superiority=0.15). Side branch late lumen loss was not significantly different between DCB and DES (–0.04 ± 0.76 vs. –0.03 ± 0.51 mm; p=0.983). An increased incidence of target lesion revascularisation (13.5% vs. 1.8%, p=0.027), mainly driven by main branch restenosis, and a numerical excess of major adverse cardiac events (17.3% vs. 7.1%, p=0.105) was found for the DES-alone strategy .
Other studies have focused on the potential benefits of DCB angioplasty for the treatment of side branches following DES implantation in the main branch. In a trial, 64 patients with bifurcation disease involving the side branch and/or the distal component of the main branch were randomly assigned to undergo predilation with DCB angioplasty of the side branch or to receive no further treatment . The postprocedural angiographic results were similar between the two groups. However, at the 9-month angiographic follow-up, the in-lesion late lumen loss (0.13±0.31 vs. 0.51±0.66; p=0.013), minimum lumen diameter (1.78±0.37 vs. 1.39±0.80; p=0.015), and binary restenosis (5.9% vs. 25.7%, p=0.045) were significantly lower in the patients who had been treated with DCB . A further small observational study tested a combined strategy for the treatment of bifurcation disease, comprising the implantation of a dedicated stent in the main branch and the application of a DCB in the side branch. This study demonstrated low late lumen loss and target lesion revascularisation at 6-month follow-up .
Bifurcation lesions treated using a DCB alone or in combination with DES, can produce comparable or superior outcomes compared with conventional DES-based strategies, but higher quality evidence is still required. Different scenarios of DCB treatment in coronary bifurcations can be conceived (Figure 9): the first is a DCB-only strategy, with DCB use in the main vessel across the side branch (SB) with or without , DCB use in the SB (‘leave nothing behind’ strategy) . Alternatively, DCBs can be used to treat the SB in the setting of a provisional bifurcation technique, either before (if planned) or after (as a bailout if required after main vessel stent) a DES is used in the main branch across the SB (blended strategy). Kissing balloon inflation with DCB should be avoided due to the time required and the proximal interaction of the two balloons which might impact on the delivery of the antiproliferative drug to the vessel wall.
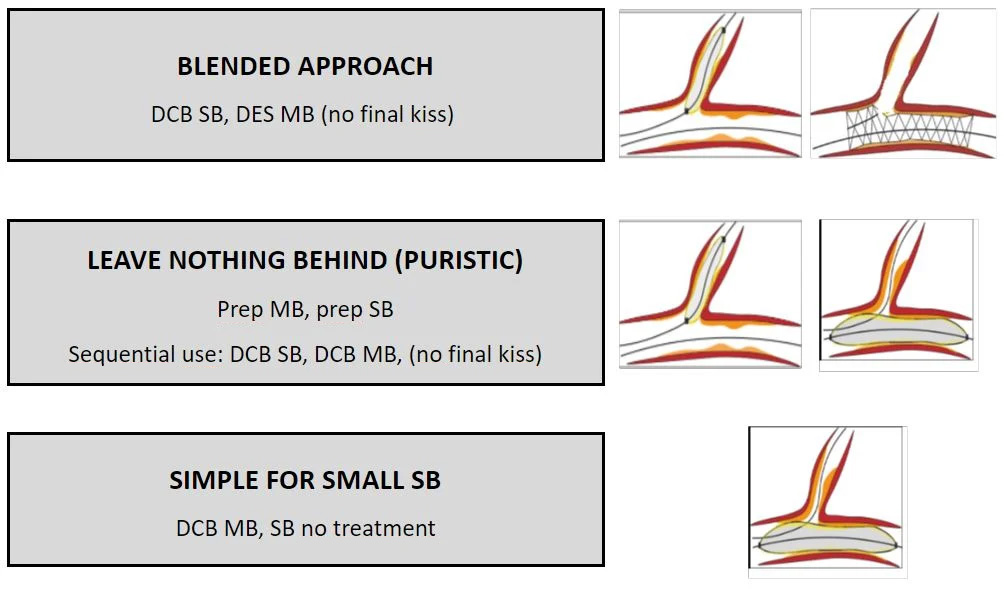
Different scenarios of DCB treatment in coronary bifurcations. DCB drug -oated balloon, DES drug-eluting stent, MB main branch, SB side branch.
A DCB-only strategy in patients presenting with ACS may be justified in coronary lesions due to plaque erosion or plaque rupture without limitation of the coronary flow. Therefore, the majority of these lesions may be adequately treated with DCB after optimal lesion preparation with preserved TIMI 3 flow. In turn, a dynamic alteration of the culprit vessel present during ACS, mainly due to vasoconstriction and thrombus burden, may lead to inappropriate sizing or apposition of the stent which have beenassociated with worse outcome. In line with this, lesions with restored normal coronary flow (TIMI 3 flow) accompanied with relief of anginal symptoms but with a suboptimal result after DCB-only PCI may be accepted as a final result that should be reassessed in the second control-angiography after a few weeks on DAPT . It should be noted that a thrombotically occluded vessel or a high thrombotic burden after lesion preparation may not be suitable for definitive treatment with DCB, as DCB do not have the ability to localise and keep the thrombus attached to the wall. Moreover, drug delivery to the vessel endothelium may be impeded by thrombus. However, in some cases, a definite differentiation between thrombus and dissection that led to the vessel closure could not be made, therefore, in such cases an initial lesion preparation with an SC balloon and reassessment thereafter are strongly recommended.
According to the PEPCAD-NSTEMI RCT, a DCB-only approach was non-inferior in comparison with BMS and DES regarding target lesion failure at 9 months in a cohort of patients with NSTEMI . In the REVELATION trial, treatment with DCB was non-inferior in comparison with DES concerning fractional flow reserve at 9 months and at two years in patients with ST-elevation myocardial infarction (STEMI) , . Results of a meta-analysis that analysed 485 patients with acute myocardial infarction (AMI) from four randomised trials support the findings that DCB is comparable to the DES in term of clinical outcome . According to the results from a large cohort of STEMI patients (1,139 patients) DCB-only treatment was comparable to DES concerning all-cause mortality after median follow-up time (>3-years) using propensity score matching analysis .
In a prespecified analysis of the BASKET-SMALL 2 RCT for cardiac death and non-fatal myocardial infarction, a significant interaction between clinical presentation and treatment was seen at one year with lower rates in patients with ACS treated by DCB. At 3 years, there were similar major adverse cardiac event rates and all-cause mortality between DCB and DES irrespective of clinical presentation, but these were higher in ACS patients compared with chronic coronary syndrome patients .
Multivessel coronary disease refers to the presence of 70% stenosis in two major coronary arteries or in one, in addition to 50% stenosis of the left main coronary artery . It can be present in up to 30-40% of all patients with coronary artery disease (CAD) . Treatment of multivessel disease may be challenging as multiple DES may be needed to address all the lesions, ending with long stent lengths. These two factors have been identified as predictors of ischaemic clinical events . Treatment with DCB may alleviate negative vessel remodelling associated with stent implantation and that lead to stent thrombosis and restenosis, without leaving any metal behind that allows for positive vessel remodelling after angioplasty , .
It has been shown that DCB-treatment approach (DCB-only or in combination with DES) in patients with multivessel disease is associated with lower stent burden and reduced mortality than a DES-only approach . In the DCB-based group, 66% of patients were treated with DCB-only, while 34% receive a DES hybrid approach. The number of stents and total stent length were significantly reduced by 65.4% and 63.7%, respectively, in the DCB-based group compared with the DES-only group. Moreover, the DCB-based group had a lower rate of MACE than the DES-only group (3.9% and 11.0%; p= p0.002) at 2-year follow-up. The DES-only group had a higher risk for cardiac death and major bleeding.
Increased bleeding risk following PCI remains a challenge as it has been associated with increased mortality, prolonged hospitalisation and higher treatment costs . Bleeding events should be classified and reported according to the Academic Risk Consortium High Bleeding Risk (ARC-HBR) criteria . Accordingly, HBR is present in case at least 1 major or 2 minor criteria are met.
The randomised DEBUT trial compared DCB-only with BMS implantation in an HBR population. Treatment of de novo lesions with DCB in patients with HBR was superior to BMS in terms of reduction of major adverse events (1.9 % vs 12.4%, respectively, p=0.003) at 9 month follow-up . Furthermore, incidence of severe bleeding was lower in the DCB-only PCI group with a shorter administration of DAPT in comparison with the group treated with DES and a standard duration of DAPT in a prespecified subgroup analysis of the BASKET-SMALL 2 trial in a cohort of HBR patients .
According to the current level of evidence, use of newer-generation of DES permits a short (1-month) duration of DAPT , . Of note, the optimal strategy concerning the number of antiplatelets used (single versus dual antiplatelet therapy) and its duration in the setting of the DCB-only PCI is still not known and remains to be elucidated in future randomised trials. The current standard of care concerning duration of DAPT after DCB-only PCI is 1-month in patients with chronic coronary syndrome. This duration of DAPT was introduced in the first RCT of DCBs for the treatment of ISR and has been used ever since . Moreover, this concept also applies for all de novo lesions , . The absence of a metallic scaffold after DCB-only PCI allows for an even shorter duration of DAPT, less than 1-month in situations of potential life-threating bleeding, without increasing ischaemic risk (i.e., early stent thrombosis) at the same time.
Diabetes is one of the major risk factors for coronary disease and it has been strongly associated with accelerated atherosclerosis, leading to premature and diffuse CAD . Furthermore, the rate of restenosis, ACS and stent-associated complications in terms of thrombosis after PCI are higher in diabetic patients compared to non-diabetic patients . According to a prespecified subgroup analysis of the BASKET SMALL 2 RCT trial, the use of DCB-only in de novo lesions in diabetes patients was non-inferior to DES in terms of MACE, however the rate of target vessel revascularisation was significantly lower with DCB than with DES (9.1% vs 15%, respectively, p=0.011 for interaction) , especially in patients treated with insulin . In one retrospective analysis, 254 patients with multivessel disease from a DCB-based PCI group were compared to the 254 propensity-matched patients treated with DES. The DCB-based group was associated with reduced MACE compared to the DES-based group in diabetic patients (HR 0.19, p=0.003), however, this was not found in non-diabetic patients (HR 0.52, p=0.167), at 2-year follow-up .
Based on the results of one meta-analysis, DCB-based PCI had lower rates of MACE, myocardial infarction, TLR and late lumen loss compared with DES-based PCI in patients with diabetes and small vessel disease .
Chronic kidney disease (CKD) with an estimated glomerular filtration rate (eGFR) <60 ml/min/1.73 m2 has been identified as an independent risk factor for death and cardiovascular events. Moreover, a positive correlation between a further reduction of eGFR and an increase of the risk for cardiovascular events has been established . Accelerated vessel calcification and profound vascular stiffness observed in these patients are triggered through disordered calcium-phosphate metabolism , .
Patients with CKD are at a higher risk of target lesion failure (OR 2.51), target vessel failure (OR 2.44) and MACE (OR 2.34) after DES-based PCI than patients without CKD at one-year follow-up . The prespecified subgroup analysis of the BASKET-SMALL 2 RCT aimed to compare the DCB-based PCI strategy to the DES-based strategy in patients with small vessel disease in the presence of chronic kidney disease (CKD), defined as estimated glomerular filtration rate <60 ml/min/1.73m2. A total of 23% (174/758) of all included patients had CKD, of whom 91 were randomised to DCB and 83 to the DES group. At 3-years follow-up, the rate of MACE was comparable between the patients treated with DCB and DES (HR 0.98, p=0.93), although the risk of all-cause and cardiac mortality was higher in patients with CKD than in those without CKD . These data confirm the safety of using DCB in this high-risk population. The use of DCB were associated with lower bleeding rates compared to DES, however this was observed irrespective of the presence of CKD. Patients with CKD are at a higher bleeding risk , , therefore a short duration of DAPT after DCB-only PCI may be a reasonable option in this subpopulation of patients with CAD.
In peripheral artery disease (PAD), DCB were about to become the standard therapy for the femoropopliteal region . However, a meta-analysis published in December 2018 reported an increased mortality in trials with 2 or 5 years of follow-up after combining treatments with paclitaxel-coated stents or DCB in peripheral artery disease . The reasons for these findings were incompletely understood as a potential underlying pathomechanism remained elusive and no relationship to the administered dose had been documented . Although the meta-analysis in peripheral arteries has considerable limitations , it has led to major uncertainty in the clinical community and raised questions about the safety of paclitaxel application in PAD. Ultimately, it was shown that the incomplete follow-up of patients and possibly, the secondary prevention approach, were not in line with the guidelines and played an important role in this misinterpretation. Subsequently, a variety of large registries and randomised studies have demonstrated the safety of paclitaxel in the treatment of PAD (174-179).
In a meta-analysis on paclitaxel DCB in the coronary arteries, we identified 26 RCTs published between 2006 and 2019 including a total of 4,590 patients. At follow-up of 6-12 months, no significant difference in all-cause mortality was found, however, with numerically lower rates after DCB treatment (risk ratio [RR] 0.74 [0.51, 1.08], p=0.116). Risk of death at 2 years (1,477 patients, 8 RCT) was similar between the two groups (RR 0.84 [0.51, 1.37], p=0.478). At 3-year follow-up (1,775 patients, 9 RCTs), all-cause mortality was significantly lower in the DCB group when compared with the control treatment group (RR 0.73 [0.53, 1.00], p=0.047) with a number needed-to-treat of 36 to prevent 1 death. A similar reduction was seen in cardiac mortality (RR 0.53 [0.33, 0.85], p=0.009) (Figure 10) .
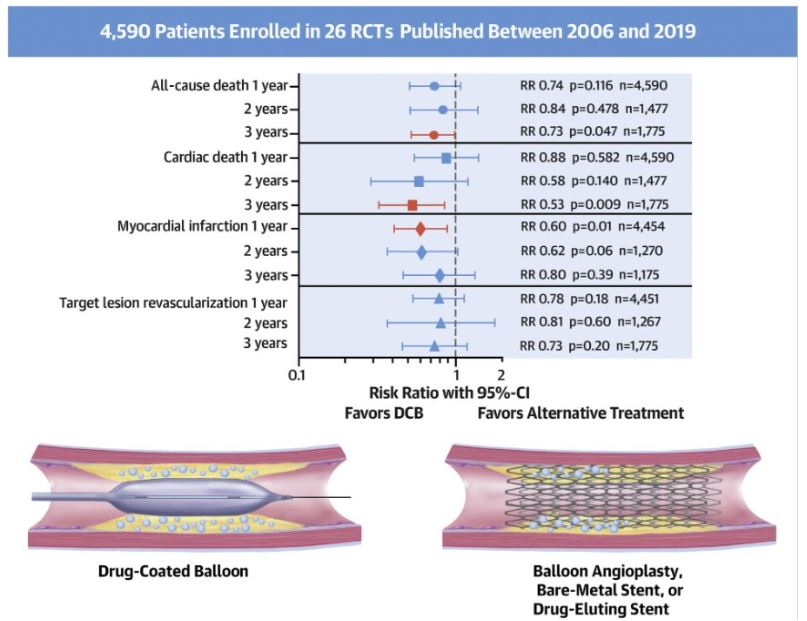
Safety of coronary paclitaxel DCB. Meta-analysis investigating the available data on survival after coronary intervention with paclitaxel-coated balloons from randomised, controlled trials. A total of 4,590 patients enrolled in 26 RCT published between 2006 and 2019 were analysed. Summary of the treatment effects for paclitaxel-coated balloon vs. alternative treatments. Relative risk of all-cause death, cardiac death, myocardial infarction, and target lesion revascularisation at one, two, and three years post-treatment. Adapted from (53).
Comparisons between first-generation paclitaxel and sirolimus DES have given rise to the doctrine that sirolimus and its analogues are the preferred drugs for local vascular therapy . However, subsequent advances in DES stent technology, such as the development of thinner-strut platforms and bioresorbable-polymer or polymer-free mechanisms of drug elution, essentially occurred in devices eluting sirolimus or its analogues , , .
Several alternative drugs to paclitaxel have been investigated . For long-term anti-restenotic efficacy, the irreversible binding of paclitaxel to microtubules resulting in long persistence in the vascular cell and favourable cell-specific effects is helpful. In contrast, sirolimus and its analogues reversibly bind to FKBP12, forming a complex with the mammalian target of rapamycin (mTOR), thus blocking cell cycle progression at the juncture of the G1 and S phases . In DES, sirolimus must be released over a period of several weeks for an effective inhibition of neointimal proliferation . Some additional challenges influence the local delivery of sirolimus DCB compared with traditional paclitaxel DCB, primarily the need for an efficient technology to transfer sirolimus into the vessel wall . Specific measures are required to facilitate a controlled drug release without having a stent platform .
Early preclinical attempts to deliver sirolimus and its analogues with the technology employed for paclitaxel DCB were unsuccessful due to insufficient tissue uptake and shorter tissue retention of -limus drugs compared with paclitaxel , . Later efforts including both nano-encapsulated sirolimus via a porous balloon and phospholipid encapsulated sirolimus nanocarriers via drug-coated balloons have resulted in a rapid decline in tissue levels , .
In a research project with different drug concentrations, additives and modifications of the crystal structure, a crystalline coating with 4 μg sirolimus per mm² balloon surface allowed for a high drug delivery and, at the same time, sufficient tissue persistence of up to 50% after 4 weeks . In an initial first-in-human randomised clinical trial of 50 patients with DES in-stent restenosis, at 6 months in-segment late lumen loss was 0.21±0.54 mm in the paclitaxel DCB group versus 0.17±0.55 mm in the sirolimus-DCB group (p=0.794) . In an extended study population of 101 patients consisting of the initial first-in-human trial and an identical trial conducted in Germany, late lumen loss (0.25±0.57 mm vs. 0.26±0.60 mm) was similar between sirolimus and paclitaxel DCB, meaning the same efficacy on neointimal proliferation . In another trial of 70 patients with de novo coronary lesions, sirolimus DCB were non-inferior to the paclitaxel DCB (0.10±0.32 mm vs. 0.01±0.33 mm) in terms of in-segment late lumen loss. In-segment late lumen enlargement was more frequent with paclitaxel DCB than sirolimus DCB (58% vs. 32%; p=0.019) .
Another commercially available sirolimus DCB is based on a nanocarrier technology of sirolimus encapsulated in a phospholipid bilayer . However, clinical evidence on this device essentially relies on mixed quality single-arm registries , . The recently published TRANSFORM I trial indicated that the MagicTouchTM sirolimus DCB did not achieve the non-inferiority primary end point of net gain when compared to the SeQuent Please Neo paclitaxel DCB, and was, in fact, inferior to this specific device . The ongoing TRANSFORM II trial will provide data on this sirolimus DCB in 1,325 patients with de novo coronary artery disease randomly assigned to sirolimus DCB or everolimus DES .
Other sirolimus DCB have been developed and may become available for clinical use in the future. Among these devices, a sirolimus DCB based on microreservoirs consisting of biodegradable polymer poly(lactic-co-glycolic acid) and sirolimus coated with a phospholipid blend (amphipathic membrane) is currently being tested in a large randomised clinical trial of 3,326 patients .
Finally, a biolimus DCB has recently shown superior 9-month angiographic late lumen loss (0.16±0.29 mm vs. 0.30±0.35 mm, p=0.001) and late lumen enlargement (29.7% vs. 9.8%, p=0.007) compared with plain balloon in the treatment of small vessel disease . Two RCTs on this type of DCB as compared with a paclitaxel DCB in the setting of ISR provided conflicting outcomes. In the REFORM trial, the biolimus DCB was clearly inferior to the paclitaxel-iopromide DCB . In contrast, Chen et al reported the results of the BIO ASCEND ISR randomised trial, in which 290 patients were enrolled at 17 sites in China, and the biolimus A9 DCB showed similar efficacy to the paclitaxel-iopromide coated balloon .
Drug-coated balloons (DCB) are gaining attraction worldwide in the treatment of peripheral and coronary lesions, especially now that the paclitaxel safety debate has been overcome. The basic prerequisite for this therapy is the best possible lesion preparation. DCBs cannot replace DES but will play an important role in the reduction of permanent implants in interventional vascular medicine in the future.
Francesco Prati, Flavio Giuseppe Biccirè
Updated on May 13, 2021
Francesco Prati, Flavio Giuseppe Biccirè, Ziad A Ali, Alessandro Sticchi, Evelyn S. Regar, Piera Capranzano
Updated on April 10, 2025
Soo-Teik Lim, Tian-Hai Koh
Updated on February 1, 2018
Scot Garg, Sharmaine Thirunavukarasu, Raffaele Piccolo, Patrick W. Serruys, Stephan Windecker
Updated on January 23, 2018